Does BSL-3 Laboratory Accreditation Exist?
March 29, 2023
More and more laboratories are built every day in countries throughout the world. Having high and maximum bio-containment laboratory capabilities is a great investment and aims for the betterment of public health. When the laboratory program, operations, and the laboratory facility is being planned, the first question you want to ask is, “What national regulations and guidelines will this laboratory meet to ensure compliance?” Identifying the laboratory standards will impact your laboratory design, biorisk management system, human resources, operations, and safety culture. Organizations want the best biosafety laboratory culture possible and want to prove that they meet or exceed in-country standards.
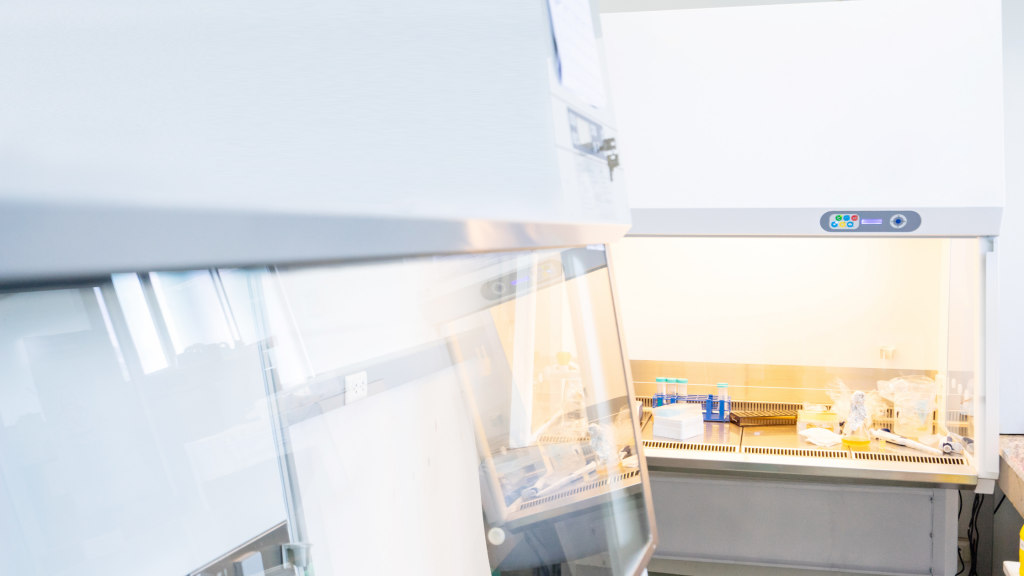
Post COVID-19, it is highly recommended that a laboratory meet a higher quality standard. World BioHazTec has been asked numerous times if a client’s high or maximum containment laboratory (BSL-3, ABSL-3, ACL-3, BSL-3Ag, BSL-4, ABSL-4) can meet an accreditation that is formally provided by an institution. At this time, there is no formal accreditation offered for biocontainment laboratories that verifies containment, capabilities, and quality, and that tests engineering and administrative controls. There are several focused accreditation programs that can be considered. Ultimately, you want a laboratory where risk can be measured as low. Guidance to attain a low-risk laboratory is achieved through meeting high or maximum containment laboratory biosafety standards such as the World Health Organization (WHO), Laboratory Biosafety Manual, Fourth Edition; CDC/NIH Biosafety in Microbiological and Biomedical Laboratories, Sixth Edition (BMBL); and NIH Design Requirements Manual. Most important is knowing the intent of these standards in their implementation. This is the first step in the process. As some organizations have prescriptive standards for accreditation, those need to be identified next. The following is a sample list of organizations with accreditation programs.
| ABSA International (The Association for Biosafety and Biosecurity) | A laboratory accreditation program has been closed. |
| AAALAC International | AAALAC International provides accreditation for organizations that use animals in research, teaching, or testing. An active animal care and use program is required to achieve accreditation. This accreditation does not apply to standard non-animal BSL-3 laboratories. |
| Clinical Laboratory Improvement Amendments | Managed by the U.S. Centers for Disease Control and Prevention (CDC), these regulations include meeting federal standards applicable to U.S. facilities or sites that test human specimens for health assessment or to diagnose, prevent, or treat disease. This certification supports clinical laboratory quality. |
| Canadian Counsel on Health Service Accreditation (CCHSA). | Accreditation of medical laboratories in Canada is regulated by provincial health authorities. Out of the ten provinces of Canada, five have provincial accreditation bodies, while in the other five provinces, medical laboratories are accredited by the Canadian Counsel on Health Service Accreditation (CCHSA). |
| The Joint Commission International | The laboratory accreditation is designed for clinical laboratories that are typically found in hospitals. High and maximum containment laboratories do not meet these criteria for accreditation due to their complex nature of design and operations. |
If you evaluate the standards and guidelines applicable to high and maximum containment laboratories, you will discover that specific language is used which does not include the word, “Accreditation.” The World Health Organization, Laboratory Biosafety Manual, Fourth Edition does not mention accreditation but offers the following definition for certification:
“Certification: A third-party testimony based on a structured assessment and formal documentation confirming that a system, person or piece of equipment conforms to specified requirements, for example, to a certain standard.” (Page xi)
The WHO goes on to state in Section 7.7.2 Audits and inspections (internal and external):
“Many laboratories implement a cooperative inspection programme where laboratory personnel are directly responsible for periodic self-audits (self-assessments) coupled with a less frequent, but more in-depth, evaluation with the biosafety officer and/or members of the biosafety committee. In some cases, laboratories may also have external audits and/or inspections, for example, as part of a certification process, under the national regulatory framework, or in an international mentoring programme. These assessments can provide information on the effectiveness of a biosafety programme, and the results can be analysed to identify weaknesses that may need to be addressed.” (Page 82)
The CDC/NIH Biosafety in Microbiological and Biomedical Laboratories, Sixth Edition (BMBL) notes:
“The BSL-3 facility design, operational parameters are verified and documented prior to operation. Facilities are tested annually or after significant modification to ensure operational parameters are met. Verification criteria are modified as necessary by operational experience.” (Page 51)
The NIH Design Requirements Manual (DRM) does not acknowledge accreditation but does provide guidance on “Critical Facility Risk Assessment and Certification” in Section 1.14:
“Certification is the systematic review of all safety features, design elements, operational modes and processes associated with a critical facility (e.g., patient care, pharmaceutical preparation, biocontainment) to validate that all facility controls and required practices (engineering controls, personal protective equipment, building and system integrity, standard operating procedures (SOPs), administrative controls such as documentation and record retention systems) are in place to minimize, to the greatest extent possible, the risks associated with operations…
Certification should be conducted before initial operation and subsequently on an annual schedule or after a program change, renovation or replacement of any engineering controls that may affect the operating environment of the facility.” (Page 90)
The aforementioned standards use words such as “certification,” “audit,” and “verification.” Accreditation is not mentioned.
The ISO 35001: Biorisk management for laboratories and other related organizations define a process to identify, assess, control, and monitor the risks associated with hazardous biological materials. However, the International Organization for Standardization (ISO) does not provide an accreditation, certification, or audit for meeting this standard.
It is the responsibility of each institution to determine if they will perform an internal certification that includes a detailed and documented risk assessment of their biosafety laboratory and program by challenging the engineering and administrative controls. Alternatively, as the WHO suggests, the institution can rely on a third-party private company to conduct the certification. If the institution trusts this responsibility to a third-party, then it is recommended to check the firm’s credentials and the professional(s)’ experience conducting the audit. Key questions for consideration include:
- Does the certifier have proven experience certifying high and maximum containment laboratories that were also inspected and approved by a government body (e.g., CDC, NIH, USDA, Canada Health, Appropriate Country Ministry of Health)? Many times, government agencies will be present to witness a certification or review the certification report. If the certifier’s documentation and report are reviewed and approved by a government agency, this demonstrates a high level of competence.
- Is the certifier properly insured? Professional liability insurance should be requested and verified. An insurance company will do their research on a certifier. They do not want to support a company or person(s) that do not have the credentials or experience. Insurance companies are vigilant in evaluating risk. If a certifier does not have professional liability insurance, then they have not been evaluated by a professional to deem them qualified enough to perform the work required in a high or maximum containment laboratory.
- Does the certifier use their own certified equipment? Engineering controls for a laboratory should be challenged. Relying on the Building Automation System to identify potential airflow issues puts the institution at risk. Certification equipment verifies if the Building Automation System is working appropriately. Ask the certifier how many differential pressure meters they possess. If they have only one or two meters, the certification testing can take days to complete. If the certifier insists on relying on just the Building Automation System, then “let buyer beware”. Ask if the equipment is calibrated to a national or international standard and request copies of each meter’s certificate of calibration to be included in the certification report. Make sure the certificates’ dates of calibration are within the certification period prescribed by the equipment’s manufacturer.
Although accreditation is an important aspect that is a part of many industries, it has not been introduced into the field of biosafety. However, certification has been utilized for decades and offers an alternative that will meet the objectives set forth in accreditation programs. Certification is more encompassing as it challenges quality processes such as administrative controls and the laboratory engineering controls. The certification process documents laboratory capabilities, risk reductions, and laboratory compliance with standards and, if applicable, accreditation programs. Lastly, certification is based upon the testing of engineering systems and documents their performance during normal and failure conditions. This is of utmost importance to ensure the containment of pathogens.
To learn more about our certification process, please visit our website. You can also book a free 30-minute consultation here or send us an email.